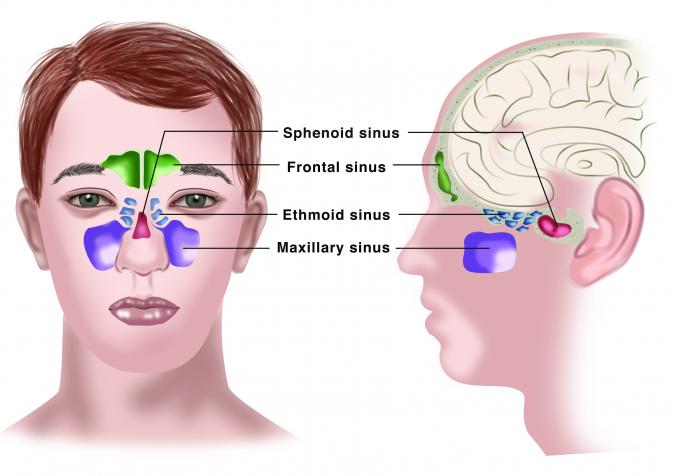
Sinuses are air-filled cavities covered by a mucosal layer and located within the bones of your face and skull.
The nose and sinuses are important for filtering, heating and moistening the air you breathe through your nose, which is an important function that protects your lungs. Sinus cavities may also contribute to voice resonance and can absorb energy to protect the brain from trauma.
Sinus diseases can be split into two categories: acute (rapid onset) or chronic (over a long period of time). Acute sinusitis is the most common form, and is characterized by a short infection or inflammation of the sinonasal mucosa, which resolves quickly after 1-2 weeks. On the other hand, chronic sinusitis symptoms last for more than 12 weeks.
Chronic sinusitis (also called chronic rhinosinusitis) is a broad diagnosis that includes different disease subtypes, further classified based on the presence of nasal polyps:
Although not fully understood, chronic rhinosinusitis is usually caused by a combination of different factors that contribute to the development of the disease. It occurs due to a malfunctional interaction between individual patient characteristics (including genes) and environmental factors. Chronic sinusitis can arise due to:
Inflammation of the sinuses is often referred to as sinusitis. However, the term rhinosinusitis is preferred to sinusitis since the inflammation of the sinuses rarely occurs without simultaneous inflammation of the nasal mucosa. Both terms are commonly used interchangeably.
Chronic sinusitis with nasal polyps runs in families but also chronic sinusitis without nasal polyps has been observed in family members, strongly suggesting that a hereditary (=genetic) factor contributes to the disease. However, studies in identical twins showed that both siblings will not necessarily develop nasal polyps, which emphasizes the additional and important role of non-hereditary, environmental factors.
In general, this is a chronic disease that cannot easily be cured, however patients sometimes have long periods of well-controlled disease. The treatment aims primarily to control patient's symptoms. Other goals are to reduce mucosal inflammation, to establish sinus drainage of secretions and to reduce sudden worsening of symptoms. Usually the disease becomes less severe after 60 years of age.
The FAQs are designed to cover more in-depth questions, particularly interesting if your condition is long-standing. If you have any questions that remain unanswered after going through this portal and FAQs, don't hesitate to contact our Team at contact@euforea.eu. Please note that we can't take any personal questions.
What is chronic rhinosinusitis (CRS)?
Inflammation is the body’s reaction to things like germs and irritants such as foreign objects or chemicals. When inflammation affects the inside lining of the nose and spreads to the sinuses, it’s called rhinosinusitis. Sinuses are the air-filled spaces above the nose. Common symptoms of rhinosinusitis include pain or pressure in the face, changes in the ability to smell, and mucus that drips out of the front part of the nose or into the back of the throat. These symptoms are in addition to the usual symptoms of rhinitis, like a stuffy/blocked nose and extra mucus in the nose.
When the symptoms of rhinosinusitis are present for more than 12 weeks, it is considered CRS. CRS can present with or without nasal polyps. Nasal polyps are soft, non-cancerous growths in the nose and/or sinuses that can cause symptoms and interfere with your daily life. To date, it remains unclear why some patients with CRS develop nasal polyps and others do not. The form of CRS with nasal polyps is also referred to as nasal polyp syndrome.
Is CRS inherited?
CRS with nasal polyps runs in families but also CRS without nasal polyps has been observed in family members, strongly suggesting that a hereditary (=genetic) factor contributes to the disease. However, studies in identical twins showed that both siblings will not necessarily develop nasal polyps, which emphasizes the additional and important role of non-hereditary, environmental factors.
Why do I have sinuses?
Sinuses are air-filled cavities in the bones of your face and skull that are covered with a thin moist layer of mucus. The nose and sinuses fulfil an important role in filtering, heating and moistening the air that we breathe through the nose. This is important to protect your lungs. The sinuses also contribute to the resonance of your voice, affecting how we sound when we speak. Moreover, the sinuses also absorb energy (“act as a cushion”) when we have an accident to protect our brain.
How many people have CRS?
Around 10% of people living in Europe have CRS. This is roughly equivalent to the entire population of Spain. In some areas of Europe, the percentage of people affected by the disease is even higher.
What is the difference between CRS and CRS?
When the inner lining of the nose becomes inflamed and the inflammation also extends to the nearby sinuses, it is called "rhinosinusitis“. Although the terms "sinusitis" and "rhinosinusitis" are often used interchangeably, rhinosinusitis more accurately describes the condition affecting both the nose and the sinuses. However, both terms are used to describe the same condition.
Does CRS progress when I get older?
CRS can change as you grow up. In kids, it’s usually milder, and nasal polyps (soft, painless growths in the nose or sinuses) don’t happen often unless the child has a condition like cystic fibrosis.
For adults, CRS with nasal polyps can get worse if it’s not treated. Over time, the polyps can grow bigger and press on the bones in the face, sometimes even changing how the face looks.
Another sign that the condition is getting worse is when asthma symptoms start to show up. These include feeling out of breath, wheezing (a whistling sound when you breathe), coughing, or bringing up mucus from your chest. If these things happen, it’s a good idea to tell your doctor.
Can CRS be cured?
CRS typically cannot be completely cured, but its symptoms can often be managed and controlled with treatment. The condition involves long-term inflammation of the sinuses which can be challenging to treat. The underlying causes of the inflammation vary and may include infections, allergies, structural abnormalities in the nose, or issues with the immune system. Usually, the disease becomes less severe after 60 years of age.
What causes CRS?
Although still not fully understood, CRS is probably caused by a combination of different factors that together contribute to the development of the disease. It is believed to be an interaction between personal traits (including your genetic code) and factors in the environment, such as air pollution, exposure to cigarette smoke or allergens. This interaction leads to a long-lasting inflammation in the sinuses and nasal cavity.
Is CRS caused by bacteria or viruses?
Inflammation is the major cause of CRS. Infections with bacteria and viruses inflame and thicken the inner lining of the sinuses and nose. This thickening hinders the removal of mucus. However, inflammation can also be caused by many other factors, such as local allergic reactions to certain bacteria and fungi. The inflammation of the sinuses can also be influenced by the presence of nasal polyps or other closely related medical conditions such as asthma, aspirin sensitivity, or immune disorders.
It is important to understand that CRS is not just an “infection that won’t clear”. Many bacteria and fungi normally live in our sinuses, whether a person suffers from sinus disease or not. While the presence of bacteria and viruses can contribute to inflammation, simply killing the bacteria with antibiotics doesn’t cure the condition. Instead, the disease likely results from a combination of different factors, including the impact from the environment and your genetics. This together produces the long-lasting inflammation that is typical in CRS.
Is CRS caused by my allergy?
The importance of allergy as a contributing factor to CRS is not fully understood. Allergies are more common among people with CRS than they are among people in the general population. This is especially true for year-round allergies to for example molds or house dust mites. Allergies that are poorly controlled can contribute to a worsening of CRS symptoms. Additionally, it appears that allergic patients get severe and recurrent CRS more often. Allergy also frequently co-exists with asthma, which further contributes to the complexity.
I think my CRS started when I inhaled some water/chemical/gas/smell via my nose at work. Is that possible?
Yes, it’s possible. Breathing in certain chemicals, gases, or contaminated water can irritate the inside of your nose and sinuses, causing inflammation. If this happens repeatedly, it can lead to long-lasting swelling and symptoms like a blocked nose or mucus buildup.
However, CRS usually happens because of several factors combined. There may be other causes, like allergies or structural problems in your nose, that you might not have noticed but also contributed to the condition.
I was very healthy until I worked at a place with poor indoor air quality. Afterwards I got the diagnosis of CRS. Did that cause my disease?
Bad indoor air quality, along with allergens like mold or dust mites, can irritate the nose and sinuses in people who are sensitive to these things. This irritation can lead to swelling and, for some, CRS, either with or without nasal polyps.
It’s hard to say for sure that poor air quality was the only cause. CRS usually happens because of several reasons coming together, like genetics, infections, or environmental factors. These things might have played a role alongside the indoor air quality.
What are the symptoms of CRS?
People with rhinosinusitis have at least two of these symptoms:
Some patients also experience ear or teeth ache, bad breath, sore throat, irritability, depression or a fatigue. Rhinosinusitis is considered chronic when the symptoms are present for at least 12 consecutive weeks.
What are the differences between a prolonged cold and CRS?
When talking about a (common) cold, we’re referring to an illness that affects your nose and throat. A cold is usually caused by a virus, and it is typically self-limiting, meaning it resolves on its own within about a week without needing medical care.
Acute rhinosinusitis, which affects both the inner lining of the nose and the nearby sinuses, often results from a viral infection associated with the common cold.
In contrast, CRS is not just ‘an infection that won’t clear’. It involves a complex interplay of your own immune system, genetics, and various environmental factors. Infections can certainly contribute to the condition or worsen it. In fact, many patients with CRS remember a nose infection as the first event of their chronic disease. However, the longstanding inflammation that is characteristic of CRS cannot be explained by infection alone. To get the diagnosis of CRS, the symptoms need to be present for at least 12 weeks in a row. In addition, confirmation of the disease is required, most often by means of a nasal endoscopy. This is a diagnostic procedure where the physician uses a camera to look inside the nose.
When should I be worried about a sinus infection not settling down?
A sinus infection caused by a virus may turn into a bacterial infection if:
Signs that the bacterial infection may be serious and need urgent care include:
If any of these symptoms occur, contact a doctor immediately for evaluation and treatment.
How will my doctor know if I have CRS?
When examining the nose, the doctor may find that the inner lining of the nose appears swollen, red, and irritated. Using a nasal endoscope, a small camera to look deeper into the nose, the doctor might also find nasal polyps or secretions coming from the sinus openings. During a throat exam, thick and colored mucus may be found dripping from the back of your nose into the throat. For some patients, the doctor may also suggest organizing a CT scan of the head. This is not necessary for all patients, but it can be helpful in case the diagnosis is less clear or when further treatment needs to be planned.
There are no specific blood tests to diagnose CRS. However, some patients may have a blood test to help in the diagnosis of a possible allergy or to rule out any immune deficiencies or autoimmune disorders.
In case of complications of CRS, one eye may show signs of swelling and redness. This will warrant further investigation by a specialist.
What are nasal polyps and what is nasal polyp syndrome?
Nasal polyps are abnormal, soft, non-cancerous growths in the nose and/or sinuses that can cause symptoms and interfere with your daily life. People with polyps often have a poor sense of smell. Patients that develop nasal polyps have a form of CRS referred to as ‘nasal polyp syndrome’ or CRSwNP (= CRS with nasal polyps).
Can nasal polyps turn into cancer if not treated well?
Nasal polyps that occur with CRS are not cancer and do not turn into cancer. However, other growths that look like polyps can form in the nasal cavity, and some of these may be cancerous or become cancerous over time.
Because of this, it’s very important to have nasal polyps checked carefully by a doctor. This is often done with a special procedure called nasal endoscopy, where a small camera is used to look inside your nose. Sometimes, other types of scans might also be needed.
Extra caution is needed if you have certain symptoms, like:
How do nasal polyps affect my health?
Small nasal polyps might not cause any symptoms at all. But when they grow larger, they can block the normal flow of mucus in your nose and sinuses. This blockage can lead to mucus buildup, which increases the chance of getting a sinus infection.
In people with CRS and nasal polyps, the swelling inside the nose can also affect the area responsible for your sense of smell (called the olfactory mucosa). This often leads to a reduced or even lost sense of smell.
Why do nasal polyps grow back?
Polyps are small, grape-like growths caused by ongoing inflammation. This inflammation makes the polyps grow and stay around, leading to symptoms like a blocked nose, mucus buildup, or trouble smelling. To lower the risk of polyps coming back, anti-inflammatory treatment with corticosteroids and rinsing with salt water are recommended.
What’s the difference between turbinates and polyps?
Turbinates are normal structures found in everyone’s nose. They are made of bone and are covered by the inner lining of the nose. Turbinates are involved in warming and adding moisture to the air you breathe, which helps protect your lungs. They can become swollen during a cold or because of allergies, but this swelling usually goes down once the cause is treated.
Polyps, on the other hand, are not normal. They are soft, non-cancerous growths that form when the lining inside the nose becomes inflamed or diseased. Polyps don’t go away on their own and can cause symptoms like a runny nose, nasal blockage, loss of smell, and a feeling of fullness or pressure in your face.
Does my lifestyle affect CRS?
Certain lifestyle factors can affect CRS. For example, exposure to cigarette smoke, irritants (including those at work), and air pollution can irritate the airways and make it harder for your nose and sinuses to clear mucus. Cigarette smoke increases the risk of airway infections. This can make it more difficult to breathe through your nose and affect your sense of smell.
CRS is also linked to acid reflux from the stomach, which some patients may have without realizing. It is recommended to limit the intake of coffee, alcohol, and acidic drinks (like soda or juice), as these can worsen acid reflux.
When I drink alcohol, I have more symptoms. I think I am allergic to it. Is that possible?
Many patients with chronic airway disease notice that their airway symptoms get worse after drinking alcohol. The exact mechanism is largely unknown, but it is not caused by an allergy. Patients often experience more severe nasal symptoms, such as a more severely blocked nose, and in some cases, alcohol can even trigger asthma attacks in those with asthma. It appears that people with CRS with nasal polyps are more likely to be sensitive to alcohol compared to those that do not have nasal polyps.
If you're looking for natural ways to reduce your symptoms, limiting alcohol, especially if you notice it triggers a reaction, can help improve symptom control.
Why do I need to stop smoking? I have been smoking for years, but my CRS just started recently.
Smoking and using any tobacco product, including e-cigarettes, cause or worsen numerous diseases. Stopping smoking is great for your overall health and can help you live longer. Smoking is a major factor causing irritation in the lungs, but also in the nose and sinuses. This irritation is a problem for all smokers but is often worse for those with CRS. You will likely have better control over your symptoms after you quit smoking.
Quitting smoking is challenging, and many people need several tries before they can stop for good. If you have decided and you are ready to quit smoking, there is lots of good help available to support you on your journey. You are more likely to be successful if you have the support from family, friends and co-workers.
Do dental problems influence CRS?
Yes, dental problems can lead to CRS. If there’s an infection in the bones around your teeth, it can spread to the sinuses, which are located just above the upper teeth. This often causesrhinosinusitis on just one side of the face.
To treat this type ofrhinosinusitis, it’s important to first fix the dental issue causing the problem. Once the dental infection is under control, your doctor can focus on treating therhinosinusitis. If you suspect your sinus problems might be related to your teeth, let your doctor and dentist know.
How much does smoking influence my nasal problems?
Smoking and being around cigarette smoke can make sinus problems worse. The smoke irritates the airways and makes it harder for your nose and sinuses to clear mucus. This can increase your chances of infections, make it harder to breathe through your nose, and reduce your sense of smell.
Active smoking might also negatively affect how well surgery works. Talk to your healthcare provider about smoking cessation as soon as possible.
What about gastric acid reflux, nutrition, and microbiological flora?
Researchers are still studying how things like stomach acid reflux (when acid from your stomach moves up into your throat), your diet, and the bacteria that naturally live in your body might impact CRS. These connections are not fully understood yet, and experts continue to study them to learn more about the impact.
What causes a runny nose?
The inflammation of the nasal and sinus mucosa leads to overproduction of nasal mucus causing the patient to experience a fullness of the nose and dripping of excess mucus out of the nose or into the throat.
What is post-nasal drip?
Post-nasal drip happens when mucus from your nose runs down the back of your throat. Normally, your nose produces about 500 ml (a small bottle’s worth) of fluid every day, and this flows into your throat in tiny droplets that you swallow without noticing.
With post-nasal drip, this normal process feels out of control. You might feel mucus building up in your throat and have the urge to swallow a lot or spit it out. Sometimes, it feels like no matter what you do, the mucus won’t clear.
For people who’ve had sinus surgery, mucus can collect in the sinuses and drain later, making post-nasal drip worse. Inflammation from CRS increases mucus production, which adds to the problem.
Using a saline rinse to flush out the mucus can help reduce the feeling of post-nasal drip and make it easier to manage.
What causes nasal blockage?
Nasal blockage happens when the lining of the nose and sinuses becomes swollen or when nasal polyps (soft growths) block the airflow. Mucus buildup and crusting can also make it harder to breathe through your nose.
Rinsing your nose with saline can help reduce swelling, clear mucus and crusts, and improve your ability to breathe.
Are my headaches caused by CRS?
Headache or facial pressure/pain is one of the main symptoms that can happen with CRS. However, if headache or facial pressure/pain is your only symptom, it’s unlikely to be caused by CRS.
Headaches related torhinosinusitis usually happen along with other symptoms like a runny nose or nasal blockage. If these symptoms are present, your headache or facial pain is more likely to be caused by CRS. Sinus headaches often feel like a dull pressure around your eyes or forehead. Headaches on the side of your head or in your neck are rarely caused by sinus problems.
An ENT doctor can check your symptoms, look inside your nose with a small camera (nasal endoscopy), and may order a CT scan to see if your sinuses are causing the headache.
Is there a way to measure headaches?
There’s no test, like a blood test or scan, that can directly measure headaches. Instead, doctors ask questions about:
This information helps doctors understand and diagnose the cause of your headache.
When should a neurologist be consulted for a headache?
If headache or facial pain is your only symptom, it’s usually not caused by sinus problems. In this case, a neurologist may need to check for neurological causes.
Other reasons to see a neurologist include:
These signs are more commonly linked to neurological conditions, and a neurologist can help figure out the cause.
I have nasal polyps, why can I not smell?
When you smell something, like a flower, tiny particles from the air travel to the upper part of your nose and interact with special smell cells called receptors in the olfactory mucosa. This area is high up inside your nose.
With CRS, especially if you have nasal polyps, inflammation affects the olfactory mucosa and reduces your ability to smell. If your polyps are large, they can physically block odors from reaching the smell receptors, making it even harder to smell.
My polyps were operated on, and they did not come back. Why do I still not smell properly?
Even after surgery to remove nasal polyps, the inflammation in your olfactory mucosa caused by CRS can remain. This ongoing inflammation can still reduce your sense of smell.
To help improve this, it’s important to keep using corticosteroid nasal sprays daily as they reduce inflammation in the smell area. In some cases, corticosteroid tablets, such as prednisolone, may temporarily improve your sense of smell, but these are usually only used for short periods due to side effects.
Will medical or surgical treatment of CRS improve my smell?
Both medical and surgical treatments aim to reduce inflammation in the nose and sinuses, which can help restore your sense of smell.
However, it’s hard to predict how much improvement you’ll see after surgery. Studies show surgery can have a positive effect, but if you stop using nasal medications afterward, your sense of smell may worsen again.
Why can I not taste?
Your sense of smell plays a big role in how you taste food. When you eat, tiny particles from the food travel through a passage connecting your throat to your nose, allowing your smell receptors to enhance the flavors.
If your sense of smell is reduced, your ability to taste can also be affected. You can try a simple experiment: pinch your nose while eating and notice how much harder it is to taste food.
Why is smell impairment difficult to treat?
The main cause of smell loss in CRS isn’t just blocked airways from swollen tissue or polyps. It’s the chronic inflammation of the olfactory mucosa. Nasal sprays containing corticosteroids can reduce this inflammation and often improve smell.
However, if the olfactory mucosa has been damaged, it may not fully recover, and your sense of smell might not return to normal.
Is there a difference in the mechanisms driving loss of smell in CRS and SARS-CoV2 infection (the virus causing COVID-19)?
Yes, the causes are different.
CRS: Smell loss happens because of chronic inflammation of the nasal and sinus lining, especially in people with nasal polyps.
COVID-19: The exact cause of smell loss is not fully understood. Researchers think it may involve temporary damage to the olfactory nerve or the cells supporting it.
Smell loss from COVID-19 often improves within a few weeks or months, but if you experience it, it’s a good idea to let your doctor know.
What impact does CRS have on sleep quality?
CRS can make it hard to sleep well. Swelling and blockages in your nose increase airflow resistance, making it harder to breathe through your nose. This often leads to mouth breathing and a buildup of nasal mucus. These issues can make it difficult to fall asleep and can cause restless or poor-quality sleep. As a result, people with CRS often feel tired and sleepy during the day.
Will surgery improve snoring and obstructive sleep apnoea?
CRS is linked to snoring and obstructive sleep apnoea (a condition where breathing stops and starts during sleep). Whether surgery can help depends on how much your sinus issues are blocking your nose and contributing to these problems. Your ENT doctor can evaluate your nasal obstruction and discuss whether surgery might improve your snoring or sleep apnoea symptoms.
What impact might CRS have on my work productivity?
CRS can affect your ability to work in two ways:
On average, people with CRS miss about 6 workdays a year. In addition, nasal symptoms like congestion, poor sleep, fatigue, and trouble concentrating can make it harder to focus and get work done, reducing overall productivity.
I have CRS and asthma. Why do my common colds take longer and are more frequent than common colds of other people?
The nose, sinuses, and lungs are all connected and affect each other. When CRS isn’t well-controlled, it can make asthma worse, and asthma can also worsenrhinosinusitis symptoms. Studies show that people with both conditions often have a weaker immune defense against viral infections, which may explain why they catch colds more frequently and why those colds last longer.
Can CRS be the cause for my chronic cough?
Yes, CRS can lead to a chronic cough. A runny nose or mucus dripping into your throat (called post-nasal drip) can irritate your throat and trigger coughing. It’s also important to test for asthma, as some coughs are caused by a type of asthma called cough-variant asthma.
What is the link between CRS and asthma?
The nose and sinuses (upper airways) and the lungs (lower airways) are closely connected. Many people with asthma also have CRS, and the more severe the asthma, the more likely it is to haverhinosinusitis, with up to 80% of severe asthma patients having CRS. Either condition can develop first, but both need to be treated together for the best results.
Why is it important to diagnose asthma in a patient with CRS?
Asthma is common in people with CRS, especially if they also have nasal polyps. Untreated asthma can make it harder to managerhinosinusitis, and both conditions often require combined treatment. For example, corticosteroids (used in inhalers for asthma and nasal sprays forrhinosinusitis) need to be carefully managed. Especially when tablets or injections are used to avoid overdosing or side effects.
Why is it important to diagnose CRS in an asthma patient?
When CRS isn’t treated, it can worsen asthma symptoms and make it harder to control. Proper treatment ofrhinosinusitis can improve asthma control, reduce symptoms, and even lower the need for strong asthma medications.
What is the link between nasal polyps, asthma and respiratory reactions to aspirin?
Some people with asthma, nasal polyps, and respiratory reactions to aspirin have a condition called aspirin-exacerbated respiratory disease (AERD), also known as Samter’s triad. About 9% of adults with asthma and 30% of adults with both asthma and nasal polyps have AERD.
AERD is not caused by taking aspirin or other NSAIDs (non-steroidal anti-inflammatory drugs), but these medications can trigger or worsen asthma and sinus symptoms. The exact cause of AERD is unknown, and it doesn’t appear to be inherited.
What impact does nasal blockage have on my lung disease?
Rhinitis (inflammation inside the nose), sinusitis (inflammation inside the sinuses) and asthma (inflammation inside the lower airways and lungs) are conditions that often coexist and can make each other worse. The nose is the air conditioner of the body and when you breathe through your nose the air is humidified and cleaned. Nasal obstruction leads to mouth breathing and the reduction of this important air conditioning function.
I have CRS. Am I at risk to get more severe COVID-19 symptoms?
Current evidence suggests that CRS does not make COVID-19 more severe. However, CRS often includes lower airway symptoms, even in people who don’t have diagnosed asthma. It’s important to stay alert for COVID-19 symptoms like loss of smell, cold- or flu-like symptoms, fever, or trouble breathing. Keeping your CRS well-controlled with treatment and following your doctor’s advice is the best way to manage your overall health.